
WHO investigating links among cough syrup deaths, considers advice for parents
WHO investigating links among cough syrup deaths, considers advice for parents
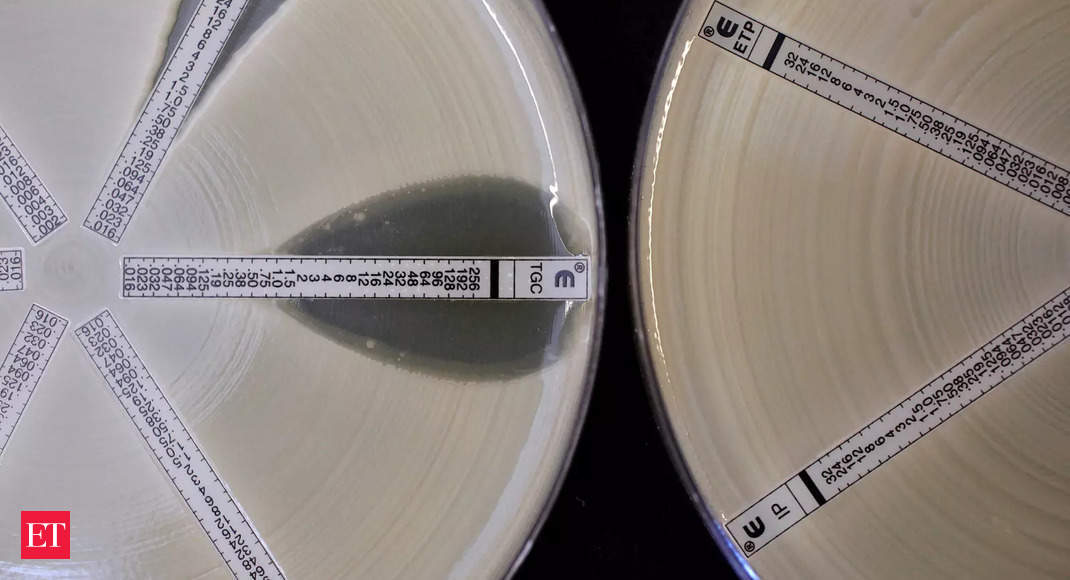
The World Health Organization (WHO) is investigating whether there is any connection between manufacturers whose contaminated cough syrups it has linked to the deaths of more than 300 children in three countries, a person familiar with the matter told Reuters. Citing “unacceptable levels” of toxins in the products, the WHO is seeking more information about the specific raw materials used by six manufacturers in India and Indonesia to produce medicines linked to the recent deaths, as well as whether the companies obtained them from some of the same suppliers, the person said. The WHO has not named any suppliers. The WHO also is considering whether to advise families globally to reassess the use of cough syrups for children in general while questions over the safety of some of these products are unresolved, the person said. WHO experts are evaluating the evidence for whether, or when, such products are medically necessary for children, the person said. The deaths of children from acute kidney injury began in July 2022 in Gambia, followed by cases in Indonesia and Uzbekistan. The WHO has said the deaths are linked to over-the-counter cough syrups the children took for common illnesses and which contained a known toxin, either diethylene glycol or ethylene glycol. To date, the WHO has identified six drugmakers in India and Indonesia who produced the syrups. These manufacturers have either declined to comment on the investigation or denied using contaminated materials that contributed to any deaths. Reuters has no evidence of wrongdoing by the companies the WHO has named. “This is of the highest priority for us, to see no more child deaths from something that is so preventable,” WHO spokesperson Margaret Harris said, without commenting further on the details of the organisation’s work. The United Nations health agency said on Monday it had widened its investigation into potential diethylene glycol and ethylene glycol contamination in cough syrups to four additional countries where the same products may have been on sale: Cambodia, the Philippines, East Timor and Senegal. It called on other governments and the global pharmaceutical industry to launch urgent checks to root out substandard medicines and improve regulation. The International Federation of Pharmaceutical Manufacturers and Associations (IFPMA) said in an emailed statement on Tuesday that its members “are already doing what the WHO is calling for”, in line with national and international guidelines. The WHO is expected to comment further on the cough syrup situation during a news conference later on Tuesday. The WHO has already issued specific alerts for cough syrups made by two Indian manufacturers, Maiden Pharmaceuticals and Marion Biotech, in October 2022 and earlier this month. It said their syrups were linked to deaths in Gambia and Uzbekistan respectively, and the alerts asked people to stop using them. Maiden and Marion’s manufacturing plants have both been shuttered. Maiden is now seeking to reopen after the Indian government said in December that its testing had found no problems with Maiden’s products. Maiden has repeatedly told Reuters, including in December, that it did nothing wrong and Managing Director Naresh Kumar Goyal said on Tuesday he had no comment on WHO investigating possible connections between the companies under scrutiny. Marion’s office phone went unanswered on Tuesday and the company did not immediately respond to an email seeking comment. Earlier this month, it told the government of Uttar Pradesh, where it is located near New Delhi, that it was being blamed for the deaths in Uzbekistan “to malign the image of India and the company”. The WHO, working with Indonesia’s drugs regulator, also issued an alert in October about cough syrups made by four Indonesian manufacturers and sold domestically. The manufacturers are: PT Yarindo Farmatama, PT Universal Pharmaceutical, PT Konimex, PT AFI Farma. PT Yarindo Farmatama, PT Konimex and PT AFI Farma did not immediately respond to requests for comment on Tuesday about the WHO investigating connections between the deaths in the three countries. PT Universal Pharmaceutical Industries’ lawyer, Hermansyah Hutagalung, said it had pulled from the market all cough syrups deemed dangerous. “Chase the suppliers, they’re the real criminals,” Hutagalung added. “They’re the ones that forge raw ingredients by falsifying raw ingredient documents all the way to pharmaceutical companies.” He did not identify specific suppliers or give details to back up the claim. The WHO said the syrups were contaminated with diethylene glycol and ethylene glycol, which it called ” toxic chemicals used as industrial solvents and antifreeze agents that can be fatal even taken in small amounts.” Their toxic effects include an inability to pass urine, kidney injury and death. The deaths have highlighted potential gaps in global regulation of commonly-used medications, including oversight of factories and supply chains, particularly those producing products for developing countries which lack the resources to monitor medicines for safety. The WHO sets guidelines on medicine manufacturing standards globally and supports countries investigating any lapses, but it has no legal mandate or enforcement authority to take direct action against violators.

First Indian intranasal Covid vaccine to be launched on Jan 26
First Indian intranasal Covid vaccine to be launched on Jan 26
Homegrown vaccine maker Bharat Biotech will launch its intranasal COVID-19 vaccine iNCOVACC, the first of its kind in India, on January 26, the company’s chairman and managing director Krishna Ella said here on Saturday. Interacting with students at the India International Science Festival in Bhopal, Ella also said that the homegrown vaccine for the lumpy skin disease in cattle, Lumpi-ProVacInd, is likely to be launched next month. “Our nasal vaccine will be officially launched on January 26, on Republic Day,” Ella said, participating in the ‘Face-to-Face with New Frontiers in Science’ segment of the IISF, organised at the Maulana Azad National Institute of Technology (MANIT). In December, Bharat Biotech had announced that it would sell the intranasal vaccine for Rs 325 per shot for procurement by the government and Rs 800 per shot for private vaccination centres.

Health should be top priority in Budget 2023, just spending isn’t enough
Health should be top priority in Budget 2023, just spending isn’t enough
It took a global pandemic to remind global leaders something that should have been clear at the outset: when it comes to healthcare, always be on the ball. Covid exposed cracks in healthcare systems, not only in low- and middle-income countries, but also in high-income countries. India, too, saw its healthcare sector stretched thin — with inadequate public health infrastructure, shortage of hospital beds, lack of emergency equipment and supplies, and limitations in data systems. According to data released by the Ministry of Health and Family Welfare, the pandemic has claimed over half a million lives in the last three years in India. With a Covid comeback remaining a very real possibility, this is not the time for the Modi government to let its guard down. Budget 2023 India may peg nominal GDP growth at about 11% i…Budget 2023 should bring tax parity between mut…The $178-billion chemical industry pins hope on…Will Budget 2023 hike threshold for tax deducti…Reading the tea leaves: The macro compulsions u…Union Budget 2023: An accelerator for electric …Union Budget 2023: The way forward for cryptocu…10 stock ideas, top themes to bet on ahead of B…The budget conundrum: How to reskill 1-billion …Urban governance reforms likely to receive push…Shaping the journey for the catalyst of India’s…Budget 2023’s twin targets: Higher capex, lower… Readers of Economic Times Online agree on the importance of healthcare spending, given the situation. In an online poll of readers ahead of the budget, almost half (47%) of the respondents said the Modi government should focus on education and healthcare — the two basic necessities — in this budget. The poll covered 5,600 ET Online readers to get their views on a host of issues the budget should tackle, including taxation, inflation and healthcare. To the question “When it comes to spending, what should the Modi government prioritise on?”, some 31% of the respondents said the government should focus on fixing the country’s creaky infrastructure; 17% said it was time to boost India’s renewable energy plans, while about 6% said defence should top the government’s priority list. ET Online The lingering threat of Covid The SARS-CoV-2 virus seems to be a never-ending threat since the pandemic broke out in 2020. Even though most of the world has gotten a grip on the pandemic that shuttered the world for almost two years, recent data from China shows that the threat is far from gone. Latest reports show China recorded 60,000 Covid-related deaths in just over a month — between December 8 and January 12. Cases have been rising in the United States, too. At least 26 cases of XBB.1.5 — the coronavirus variant behind the surge in Covid cases in the US — have been found in India so far. The variant has been found in 11 states and Union territories till now, including Delhi, Maharashtra and West Bengal. Given this situation, the ET Online poll asked its readers what measures India should take if the Covid situation worsens. Nearly half of the respondents said the government should ensure availability of all medical facilities and also foot the bill. In the wake of the pandemic, a significant budgetary increase for the healthcare sector had pushed India’s health expenditure to 2.1% of GDP for the first time in 2021-22, bringing it close to the government’s policy aspiration. This is within touching distance of the government’s healthcare expenditure target of 2.5% of GDP by 2025, as envisaged in the National Health Policy, 2017. On if another lockdown would be viable in case the situation deteriorates, 40% of the respondents voted against the idea, saying that the government should keep mobility options open so that travel and transportation would not be hindered; 5.8% said another national lockdown would be a good idea. An almost equal number of the respondents were of the opinion that the Modi government should announce more fiscal measures with direct cash transfers. ET Online Boosting healthcare When asked about boosting healthcare in the country, two things stood out. While 43% of the respondents said that the government needed to increase its budgetary outlay to fix the healthcare sector, 47% said more than increasing the funds, the government should focus on successful implementation of its policies. India has learnt from the pandemic and introduced initiatives to ramp up response and manage future health emergencies. In an article in ET Online, Kaustabh Basu, Partner-Social Sector, PwC India, pointed out such moves. “The launch of the Aarogya Setu application during the Covid-19 outbreak allows communities to participate in disease surveillance. Furthermore, initiatives such as the Pradhan Mantri-Ayushman Bharat Infrastructure Mission (PM-ABHIM), National Digital Health Mission (NDHM), One Health Consortium and Integrated Health Information Platform (IHIP) are also steps taken to prepare better for health emergencies,” Basu said. The pharmaceutical industry has proven to be a dependable partner during the Covid crisis by ensuring there was access to adequate countermeasures. “With the roll out of schemes for strengthening the pharmaceuticals industry, the country is well-placed to incorporate measures for manufacturing preparedness and response for health emergencies,” Basu added. ET Online

Gearing up for the future: Strengthening India’s pandemic preparedness and response
Gearing up for the future: Strengthening India’s pandemic preparedness and response
The relevance of pandemic preparedness and the need for having an appropriate response has increased owing to the COVID-19 pandemic, an infectious disease which, as of January 2023, has claimed more than six million lives and infected more than 660 million people, globally (World Health Organization COVID-19 Dashboard). In India, the pandemic has claimed over half a million lives in the last three years (Ministry of Health and Family Welfare, Government of India). The pandemic occurred amid the implementation of the Sustainable Development Goals (SDGs) and has significantly impacted the progress on achieving the targets. While the rise in extreme poverty due to COVID-19 will lead to missing the targets set for eradicating poverty (SDG 1), the progress on SDG 3 ‘good health and wellbeing’ has also reversed. The second SDG of a hunger-free world will be missed, with nearly 660 million people facing acute food shortages due to COVID-19 impact (World Economic Forum 2021). This humanitarian crisis and its resultant socio-economic impact has highlighted the need to redesign and strengthen the approach to prepare for future health emergencies, especially pandemics. The pandemic exposed the fragility of health systems across the globe; high income countries were as much impacted as low and middle-income countries. The Indian health system was stretched too, due to inadequate public health infrastructure, shortage of hospital beds, lack of emergency equipment and supplies (such as ventilators and oxygen), and limitations in data systems for effective decision making. The global community, taking lessons from the COVID-19 pandemic, has initiated steps in this direction. The Organization for Economic Cooperation & Development’s policy response ‘Building back better’ to not only getting economies and livelihoods back on track, but also safeguarding prosperity for longer term and World Health Organization (WHO)’s ten proposals to strengthen the global architecture for health emergency preparedness, response, and resilience (HEPR) are a welcome move. The recent launch of the Pandemic Fund by the World Bank is another initiative to promote pandemic preparedness and response. Although there are numerous institutions and financing platforms that aid activities in this direction, this would be a platform solely focused on providing critical financial investments to strengthen required capacities at national, regional, and global level. India, too, has taken initiatives to ramp up the whole-of-the-government and whole-of-society response to manage future health emergencies in a more agile and efficient manner. The launch of the Aarogya Setu application during the COVID-19 outbreak allows communities to participate in disease surveillance. Furthermore, initiatives such as the Pradhan Mantri- Ayushman Bharat Infrastructure Mission (PM-ABHIM), National Digital Health Mission (NDHM), One Health Consortium and Integrated Health Information Platform (IHIP) are also steps taken to prepare better for health emergencies. While PM-ABHIM focuses on strengthening healthcare systems through enhanced capacity of National Centre for Disease Control, establishment of health and wellness centres and network of laboratories, One Health Consortium aims to initiate cross-cutting collaborations between animal, human and environmental health. India has also signed up to WHO’s ‘Triple Billion targets by 2023’, a measurement and policy strategy to ensure that, globally, one billion more people benefit from the universal health coverage, and are protected from health emergencies, so they can enjoy better health and wellbeing. In addition to these initiatives, certain other critical elements would also require dedicated efforts to strengthen India’s pandemic preparedness and response. Strengthening private sector participation, leveraging digital systems, engaging pharmaceutical industry, and increasing government expenditure on health as percentage of the Gross Domestic Product (GDP) are expected to have far reaching gains in India’s strategy to be future ready for any health emergency. As per the national health estimate 2018-19, the current health expenditure (% of GDP) in India is at 3.16 per cent of which the government health expenditure is only 1.28 per cent. This is far from the target of 2.5 per cent of government expenditure on health (National Health Policy 2017) and hence, needs to be increased. Though the private health sector caters to nearly three-fourth of out-patient load in India, their participation on some of the components of health emergency preparedness and response remain low. Mechanisms to engage private sector in providing hospital and diagnostic resources and initiating newer service delivery platforms should be explored, along with enhancing their participation in disease surveillance. With the explosion of digital health technologies in India, digital innovations are the way forward to unify and integrate the plethora of health-related data platforms. Measures like linking morbidity and mortality data to help estimate disease burden by geographies and integration of Integrated Health Information Platform with National Animal Disease Reporting System (NADRS), to ensure integrated reporting under One Health, can help translate data into meaningful and timely response plan. The pharmaceutical industry has proven to be a dependable partner during the COVID-19 crisis by ensuring an adequate access to counter measures within the country. It has also lent a helping hand to the partner nations, which should be further leveraged for pandemic preparedness and response. With the roll out of schemes for strengthening the pharmaceuticals industry, the country is well-placed to incorporate measures for manufacturing preparedness and response for health emergencies. With India taking over the G20 presidency, the national government has highlighted tackling health emergencies as one of the three focus areas for the health working group. This will require dedicated efforts by India to leverage global partnerships for pandemic preparedness and response, and will also drive India’s approach to become the voice of the global south. (The author is a Partner – Social Sector at PwC India)

Gearing up for future: Strengthening India’s pandemic preparedness and response
Gearing up for future: Strengthening India’s pandemic preparedness and response
The relevance of pandemic preparedness and the need for having an appropriate response has increased owing to the COVID-19 pandemic, an infectious disease which, as of January 2023, has claimed more than six million lives and infected more than 660 million people, globally (World Health Organization COVID-19 Dashboard). In India, the pandemic has claimed over half a million lives in the last three years (Ministry of Health and Family Welfare, Government of India). The pandemic occurred amid the implementation of the Sustainable Development Goals (SDGs) and has significantly impacted the progress on achieving the targets. While the rise in extreme poverty due to COVID-19 will lead to missing the targets set for eradicating poverty (SDG 1), the progress on SDG 3 ‘good health and wellbeing’ has also reversed. The second SDG of a hunger-free world will be missed, with nearly 660 million people facing acute food shortages due to COVID-19 impact (World Economic Forum 2021). This humanitarian crisis and its resultant socio-economic impact has highlighted the need to redesign and strengthen the approach to prepare for future health emergencies, especially pandemics. The pandemic exposed the fragility of health systems across the globe; high income countries were as much impacted as low and middle-income countries. The Indian health system was stretched too, due to inadequate public health infrastructure, shortage of hospital beds, lack of emergency equipment and supplies (such as ventilators and oxygen), and limitations in data systems for effective decision making. The global community, taking lessons from the COVID-19 pandemic, has initiated steps in this direction. The Organization for Economic Cooperation & Development’s policy response ‘Building back better’ to not only getting economies and livelihoods back on track, but also safeguarding prosperity for longer term and World Health Organization (WHO)’s ten proposals to strengthen the global architecture for health emergency preparedness, response, and resilience (HEPR) are a welcome move. The recent launch of the Pandemic Fund by the World Bank is another initiative to promote pandemic preparedness and response. Although there are numerous institutions and financing platforms that aid activities in this direction, this would be a platform solely focused on providing critical financial investments to strengthen required capacities at national, regional, and global level. Budget 2023 Will Budget take a pause on bank privatisation?What income tax relief Budget can give for midd…Urban governance reforms likely to receive push…Will Budget hike threshold for TDS on income fr…Fiscal deficit an important variable to track i…India may peg nominal GDP growth at about 11% i…Budget 2023 should bring tax parity between mut…Budget 2023 expected to focus on job creationThe $178-billion chemical industry pins hope on…Reading the tea leaves: The macro compulsions u…Union Budget 2023: An accelerator for electric …Union Budget 2023: The way forward for cryptocu… India, too, has taken initiatives to ramp up the whole-of-the-government and whole-of-society response to manage future health emergencies in a more agile and efficient manner. The launch of the Aarogya Setu application during the COVID-19 outbreak allows communities to participate in disease surveillance. Furthermore, initiatives such as the Pradhan Mantri- Ayushman Bharat Infrastructure Mission (PM-ABHIM), National Digital Health Mission (NDHM), One Health Consortium and Integrated Health Information Platform (IHIP) are also steps taken to prepare better for health emergencies. While PM-ABHIM focuses on strengthening healthcare systems through enhanced capacity of National Centre for Disease Control, establishment of health and wellness centres and network of laboratories, One Health Consortium aims to initiate cross-cutting collaborations between animal, human and environmental health. India has also signed up to WHO’s ‘Triple Billion targets by 2023’, a measurement and policy strategy to ensure that, globally, one billion more people benefit from the universal health coverage, and are protected from health emergencies, so they can enjoy better health and wellbeing. In addition to these initiatives, certain other critical elements would also require dedicated efforts to strengthen India’s pandemic preparedness and response. Strengthening private sector participation, leveraging digital systems, engaging pharmaceutical industry, and increasing government expenditure on health as percentage of the Gross Domestic Product (GDP) are expected to have far reaching gains in India’s strategy to be future ready for any health emergency. As per the national health estimate 2018-19, the current health expenditure (% of GDP) in India is at 3.16 per cent of which the government health expenditure is only 1.28 per cent. This is far from the target of 2.5 per cent of government expenditure on health (National Health Policy 2017) and hence, needs to be increased. Though the private health sector caters to nearly three-fourth of out-patient load in India, their participation on some of the components of health emergency preparedness and response remain low. Mechanisms to engage private sector in providing hospital and diagnostic resources and initiating newer service delivery platforms should be explored, along with enhancing their participation in disease surveillance. With the explosion of digital health technologies in India, digital innovations are the way forward to unify and integrate the plethora of health-related data platforms. Measures like linking morbidity and mortality data to help estimate disease burden by geographies and integration of Integrated Health Information Platform with National Animal Disease Reporting System (NADRS), to ensure integrated reporting under One Health, can help translate data into meaningful and timely response plan. The pharmaceutical industry has proven to be a dependable partner during the COVID-19 crisis by ensuring an adequate access to counter measures within the country. It has also lent a helping hand to the partner nations, which should be further leveraged for pandemic preparedness and response. With the roll out of schemes for strengthening the pharmaceuticals industry, the country is well-placed to incorporate measures for manufacturing preparedness and response for health emergencies. With India taking over the G20 presidency, the national government has highlighted tackling health emergencies as one of the three focus areas for the health working group. This will require dedicated efforts by India to leverage global partnerships for pandemic preparedness and response, and will also drive India’s approach to become the voice of the global south. The author is Partner – Social Sector, PwC India.

Budget 2023: Top 5 things India’s healthcare sector is craving for
Budget 2023: Top 5 things India’s healthcare sector is craving for
The Indian Healthcare Sector requires a comprehensive sector development program under the government of India to foster private sector investment, medical education infrastructure development, support structured financing at low cost, drive digitization in the healthcare sector, a roadmap towards universal healthcare coverage, and cohesive efforts of private and public sector towards building a “Healthy India”. Union Budget 2022-23, the Government of India allocated around Rs 86,200 Cr to the Ministry of Health and Family Welfare (MoHFW) 16.5 percent increase compared to the previous year. The Union Budget 2023-24 for the healthcare sector should be drafted keeping in mind the long-term vision for building a “Healthy India” with sustainable healthcare infrastructure and healthcare workforce. There is a need to increase the budget by a minimum of 30 to 35 percent focusing on the below five priority areas: Health Insurance of India’s Missing Middle– Comprehensive insurance model to cover the missing population – In 2021, as highlighted by the Niti Aayog report titled “Health Insurance of India’s Missing Middle”, a population of around 40 crore individuals are still devoid of any financial protection. Although in 2022, the government took the initiative of extending AB-PMJAY cover to senior citizens (women above the age of 65 and men above 75 years) but still, there is an urgent need for developing health coverage and financing models under AB-PMJAY to provide mandatory health coverage to rest of the missing population. Establishing a healthcare infrastructure fund – Micro, Small and Medium Enterprises (MSMEs), startups, and Medical Device parks are some of the areas in which the government has set up dedicated funds and schemes to support infrastructure development.In the last few years, there have been fewer new medical colleges in the private sector, and the recent capping on fees has further limited the interest of the private sector to set up medical colleges. Central and state governments can establish a healthcare fund to provide them with low-cost capital, support with dedicated viability gap funding for PPP projects, subsidies for medical equipment, and financial benefits such as land at a concessional rate for development of projects across Tier-II and Tier-III cities. Tax benefits for healthcare skilling and development – As per the Income Tax Act, 2013-Section 35CCD, for computing business income, a manufacturing company is allowed a weighted deduction of 150 percent of expenses (other than land or building) incurred on a skill development project, allowing manufacturers to recover the money invested on the skill development needed for their industry. These fees may also be repaid to the company in cash returns rather than tax deductions. To be eligible, employees must take six months or more to complete a training programme before starting full-time employment. This provision should be amended and offered to healthcare organisations (hospitals and diagnostic companies) for apprentice training of healthcare professionals. Tax benefits on preventive health check-ups – Government should increase the health checkup deduction limit of ₹5,000 to ₹15,000 for a family in the budget 2023 to encourage citizens towards preventive health check-ups. Incentivization for digitization in the healthcare sector – Providers who leverage the digital transformation journeys such as the adoption of telemedicine/virtual care solutions, referral management systems, Personal Health Records/Electronic Health Records (PHR/ EHR) could leverage the subsidies and/or indirect tax incentives for capital and operational expenses. The country is recovering from the aftereffects of the pandemic and growing demand for healthcare services has underlined the need for more budgetary allocation in the healthcare sector to enhance the patient experience, attract smart investments in relevant digital health technologies, augment healthcare infrastructure, establish an ecosystem through collaboration, and develop an agile but robust governance structure. (The author is a Partner and Co-head of Healthcare at KPMG in India)

Over 1.54 lakh sub, primary health centers transformed into Ayushman Bharat-Health and Wellness Centers: Mansukh Mandaviya
Over 1.54 lakh sub, primary health centers transformed into Ayushman Bharat-Health and Wellness Centers: Mansukh Mandaviya
More than 1.54 lakh sub health centres and primary health centre in the country have been transformed into Ayushman Bharat-Health and Wellness Centres, exceeding the target of starting 1.50 lakh AB-HWCs by December 31 last year, Union Health Minister Mansukh Mandaviya said on Thursday. Mandaviya, who chaired the eighth meeting of Mission Steering Group (MSG) of National Health Mission (NHM) here, also said that the HWCs have witnessed more than 135 crore footfall since 2018, according to a statement from the health ministry. “For the first-time health is being linked with the agenda of development under a holistic approach undertaken by the union government. The pandemic period has provided us an opportunity to strengthen our healthcare infrastructure and delivery systems,” Mandaviya said. The MSG is the apex decision-making body of NHM that takes decisions on policies and program implementation under the Mission. Minister of Housing and Urban Affairs Hardeep Singh Puri, Union Minister of Jal Shakti Gajendra Singh Sekhawat, Union Minister of Social Justice and Empowerment Dr Virendra Kumar, Minister of State for Health Bharati Pravin Pawar and NITI Aayog member (Health) were also present. Highlighting the achievements under NHM, Mandaviya said: “Exceeding the target of 1.50 lakh AB-HWCs by December 31, 2022, more than 1.54 lakh Sub Health Centres and Primary Health Centres have been transformed as AB-HWCs. In sync with the approach of the National Health Policy 2017 (NHP 2017), AB-HWCs are providing comprehensive primary healthcare closer to the communities. As many as 12 health services packages are available free-of-charge”. Mandaviya stressed that while we need to understand global healthcare systems and their best practices, India can have its own healthcare model which would be aligned to its regional requirements, and customised to the local strengths and challenges. Moving with the philosophy of Antyodaya, the Government aspires to provide affordable, accessible and quality healthcare services to each individual in every corner of the country, he emphasised, the statement said. The MSG was informed about the ‘Holistic Approach’ adopted by NHM encompassing change in programme design to respond to changing health care needs. The MSG was apprised about the achievements made under NHM during the past few years according to which 1 lakh AB- HWCs have started providing teleconsultation services through the e-Sanjeevani platform and technical specification and draft guidelines of HPV vaccine has been approved. The MSG was further informed that 30 Crore ABHA IDs have been created so far and integrated with the National Digital Healthcare Ecosystem, and around 20 crore AB-PMJAY cards have been created as well. The Pradhan Mantri National Dialysis Program (PMNDP) has been implemented in 630 districts of 36 states and Union Territories. Besides, tertiary services are gradually being provided in district hospitals as well, and over 9 lakh TB patients adopted under the Nikshay Mitra initiative. Commending the progress under the Nikshay Mitra initiative, the union health minister emphasised on the need to eradicate Tuberculosis (TB) by 2025 as per Prime Minister’s vision of achieving the target of TB Elimination target by the year 2025. The MSG also deliberated upon increasing focus towards preventive and promotive health approach that advocates for a holistic wellness outlook in the community.

Budget 2023: Healthcare tech industry body seeks cut in customs duty, removal of health cess on medical devices
Budget 2023: Healthcare tech industry body seeks cut in customs duty, removal of health cess on medical devices
Ahead of the Budget, Medical Technology Association of India (MTaI) on Wednesday urged the government to reduce customs duties and removal of health cess on imported medical devices. MTaI, which represents medical technology companies, appreciated the various reforms undertaken by the government during the previous year, but said that more was needed to be done as 80 per cent of the medical devices used are imported. MTaI Chairman and Director General Pavan Choudary said the customs duties and taxes levied on medical devices in India are one of the highest in the world and highest among the neighbouring countries which directly impacts patients’ affordability. “As the preparation for the Union Budget 2023 gets underway, we expect a correction in the customs duties and taxes levied on medical devices,” Choudary said. The sector, he added, requires more focus in government outlays and one way to achieve this is by increasing the public health spending to meet the current gaps in healthcare demand and supply. He also suggested the government should consider a separate budget allocation for promoting and marketing medical device sector globally. Budget 2023 Will Budget take a pause on bank privatisation?What income tax relief Budget can give for midd…Urban governance reforms likely to receive push…Will Budget hike threshold for TDS on income fr…Fiscal deficit an important variable to track i…India may peg nominal GDP growth at about 11% i…Budget 2023 should bring tax parity between mut…Budget 2023 expected to focus on job creationThe $178-billion chemical industry pins hope on…Reading the tea leaves: The macro compulsions u…Union Budget 2023: An accelerator for electric …Union Budget 2023: The way forward for cryptocu… MTaI said the high customs duty has adversely impacted the costs of medical devices in India and it should be reduced to 2.5 per cent. Also, the 5 per cent health cess ad valorem imposed on imported medical devices has further compounded the burden on the industry and should be removed. There is a need for focussed increase in public spending on health infrastructure especially in Tier 2, Tier 3 cities and rural areas, MTaI added. Finance minister Nirmala Sitharaman will unveil the Budget for 2023-24 on February 1.

HLL pays Rs 122.47 cr as dividend to Health ministry for FY 2021-22
HLL pays Rs 122.47 cr as dividend to Health ministry for FY 2021-22
HLL Lifecare Limited (HLL), a mini-ratna public sector enterprise under Union Ministry of Health & Family Welfare, on Wednesday paid a dividend of Rs 122.47 crore to the Health Ministry for financial year 2021-22. Expressing happiness at the record turnover of Rs 35,668 crore and a profit before tax of Rs 551.81 crore of HLL during the financial year 2021-22 and appreciating their support during the pandemic, Mandaviya said, “HLL has played an important role in the procurement and distribution of emergency medical supplies supporting the Union Health Ministry for Covid- 19 pandemic management. As a nodal agency for procurement and supply of emergency medical items for COVID-19 pandemic management, it has enabled real time management of the crisis”. HLL Chairman & Managing Director Beji George presented the cheque to Union Health Minister Mansukh Mandaviya in presence Dr Bharati Pravin Pawar, MoS(HFW) at a function held at Nirman Bhavan, here. Speaking on the occasion, Mandaviya said that though PSUs were established with great vision, their performance has not always been satisfactory. Expressing concerns over sustainability of PSUs, he pointed out that “financial discipline and responsible behaviour are key aspects for the sustainability of PSUs.” Dr Pawar also congratulated HLL for their achievement and lauded its efforts during the pandemic. HLL was incorporated on March 1, 1966 to produce contraceptives to support Government’s family planning programme. While focusing and expanding the core areas like reproductive healthcare, HLL diversified into other healthcare segments like hospital products, hospital infrastructure management, medical equipment procurement consultancy, diagnostic services, retailing of pharmaceuticals etc.
Urgent need to develop antibiotics for newborns, say global experts
Urgent need to develop antibiotics for newborns, say global experts
There is an urgent need to develop antibiotics for newborn babies, a population that is particularly vulnerable to antibiotic resistance, according to leading global public health experts including those from India. Recent estimates show about 2.3 million newborns die of severe bacterial infections each year while an increasing number are becoming resistant to currently used antibiotics, the experts said in a report published in the December 2022 Bulletin of the World Health Organization. Over the last decade, AMR has worsened to the point where around 50-70 per cent of common pathogens show a high degree of resistance to available first and second-line antibiotics, they said. The paper is co-authored by international experts in the field of antimicrobial resistance (AMR), including those from the Global Antibiotic Research & Development Partnership (GARDP) and All India Institute of Medical Sciences (AIIMS). The authors noted that despite substantial progress in medical research and a steep decline in the number of children under the age of five who die of preventable diseases, many problems related to child health remain to be tackled. Severe bacterial infections are one of them. “There is an urgent need to identify high priority antibiotics to understand which ones work best and safely in children, and then make them available where they are needed,” said Mike Sharland from St George’s, University of London (SGUL), and member of the Antimicrobial Resistance Programme at Penta – Child Health Research. “By achieving global consensus, we can streamline the process of antibiotic development, allow for faster access to antibiotics, and reduce the burden of AMR on the vulnerable neonatal population,” added Manica Balasegaram, Executive Director of GARDP. The report also highlights how collaborative antibiotic development and access network specifically targeting newborns could also prove valuable compared to single independent studies. A successful example, the authors noted, has been the collaboration between GARDP, Penta – Child Health Research, SGUL, and other partners on a recent global observational study of 3,200 babies with neonatal sepsis across 19 hospitals in 11 countries. They are also partnering on an upcoming clinical trial, which will start in South Africa within the next few months before being expanded to other countries. Despite a rising number of newborn deaths caused by AMR, very few effective antibiotics have been adequately studied to treat serious bacterial infections such as neonatal sepsis, the authors said. As many as 40 antibiotics approved for use in adults since 2000, only four have included dosing information for newborns in their labels, they said. According to the report, ethical concerns, logistical issues and regulatory requirements have made it difficult to conduct clinical research in newborns. There is a long delay in completing paediatric regulatory studies and they are also not harmonised globally to demonstrate clinical utility in newborns, it said.
